Maternal and Fetal Nutrition - ppt download
Learning Objectives Discuss recommendations for maternal weight gain during pregnancy. Compare the recommended level of intake of energy sources, protein, and key vitamins and minerals during pregnancy and lactation. Give examples of the food sources that provide the nutrients required for optimal maternal nutrition during pregnancy and lactation. Examine the role of nutritional supplements during pregnancy. List nutritional risk factors during pregnancy. Analyze examples of eating patterns of women from two different ethnic or cultural backgrounds, and identify potential dietary concerns. Assess nutritional status during pregnancy. Discuss nutritional considerations for pregnant women who are obese and those who have had bariatric surgery. Describe food safety precautions for pregnant women.
Chapter 15. Maternal and Fetal Nutrition. Copyright © 2016 by Elsevier Inc. All rights reserved.
Compare the recommended level of intake of energy sources, protein, and key vitamins and minerals during pregnancy and lactation. Give examples of the food sources that provide the nutrients required for optimal maternal nutrition during pregnancy and lactation. Examine the role of nutritional supplements during pregnancy. List nutritional risk factors during pregnancy. Analyze examples of eating patterns of women from two different ethnic or cultural backgrounds, and identify potential dietary concerns. Assess nutritional status during pregnancy. Discuss nutritional considerations for pregnant women who are obese and those who have had bariatric surgery. Describe food safety precautions for pregnant women.
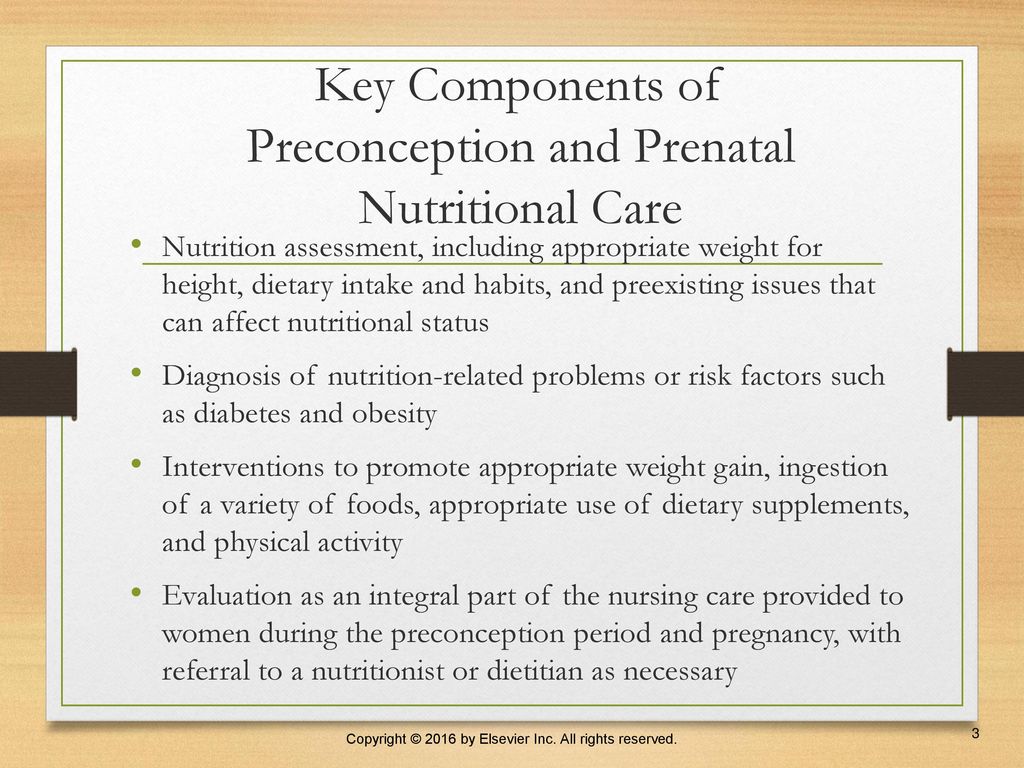
Nutrition assessment, including appropriate weight for height, dietary intake and habits, and preexisting issues that can affect nutritional status. Diagnosis of nutrition-related problems or risk factors such as diabetes and obesity. Interventions to promote appropriate weight gain, ingestion of a variety of foods, appropriate use of dietary supplements, and physical activity. Evaluation as an integral part of the nursing care provided to women during the preconception period and pregnancy, with referral to a nutritionist or dietitian as necessary.
Healthy diet ensures adequate nutrients for developing fetus. First trimester critical in terms of embryonic and fetal development. Folic acid intake. 0.4 mg in fortified foods recommended. Neural tube defects can occur with poor intake. Desirable body weight reduces maternal and fetal risks.
Dietary reference intakes (DRIs) Energy needs. Body mass index. Weight gain. Pattern of weight gain. Hazards of restricting adequate weight gain. Excessive weight gain. Protein. Fluids.
Omega-3 fatty acids. Fluids. Minerals and vitamins. Iron. Physiologic anemia. Calcium. Magnesium. Sodium. Potassium. Zinc.
Minerals and vitamins (Cont.) Fat-soluble vitamins. Water-soluble vitamins. Folate and folic acid. Vitamin C. Vitamin B6. Vitamin B12. Multivitamin-multimineral supplements during pregnancy.
Alcohol. There is no safe amount or type of alcohol during pregnancy, and there is no time during pregnancy when alcohol consumption is without risk. Caffeine. Data unclear. General recommendation of no more than 200 mg of caffeine a day. Artificial sweeteners. Pica and food cravings.
Adolescent pregnancy needs focus on improving. Nutrition knowledge. Meal planning. Food preparation. Access to prenatal care. Nutritional interventions. Educational programs. Physical activity during pregnancy. Factors to consider prior to exercise. Dehydration. Calorie intake.
Obstetric and gynecologic effects on nutrition. Diet history. Health history. Usual maternal diet. Physical examination. Anthropometric (body) measurements. Laboratory testing. Anemia.
Programs for women with limited financial resources. SNAP. WIC. Daily food guide and menu planning. MyPlate program. Food safety. Medical nutrition therapy.
Nutrition-related concerns during pregnancy. Iron supplementation. Nutrition-related discomforts of pregnancy. Nausea and vomiting. Constipation. Heartburn (pyrosis)
Vegetarian diets. Consuming a variety of different plant proteins—grains, dried beans and peas, nuts, and seeds—on a daily basis can provide all of the essential amino acids. Cultural influences. Nurse should be aware of what constitutes a typical diet for each cultural or ethnic group.
Appropriate weight loss goals. Nonlactating women—0.5 to 0.9 kg per week. Lactating women—1 kg per month. Attain a healthy weight. Weight loss and breastfeeding.
Similar to those during pregnancy. Needs for energy, protein, vitamins, minerals are greater than nonpregnant needs. The recommended energy intake for the first 6 months PP is 330 kcal more than nonpregnant intake. The AAP recommends that breastfeeding women who are well nourished should add 450 to 500 kcal/day to a balanced diet. Adequate fluid intake. Avoid smoking, alcohol, and excessive caffeine.
A woman’s nutritional status before, during, and after pregnancy contributes, to a significant degree, to her well-being and that of her developing fetus and newborn. Many physiologic changes occurring during pregnancy influence the need for additional nutrients and the efficiency with which the body uses them. Both the total maternal weight gain and the pattern of weight gain are important determinants of the outcome of pregnancy.
The appropriateness of the woman’s prepregnancy weight for height (BMI) is a major determinant of her recommended weight gain during pregnancy. Nutritional risk factors include adolescent pregnancy; abuse of nicotine, alcohol, or drugs; bizarre or faddish food habits; a low or high weight for height; and frequent pregnancies. Iron supplementation is usually routinely recommended during pregnancy. Other supplements may be warranted when nutritional risk factors are present.
Women who are pregnant should consume seafood that is low in methylmercury. The nurse and the pregnant woman are influenced by cultural and personal values and beliefs during nutrition counseling.
Dietary modifications can be effective interventions for some of the common discomforts of pregnancy, including nausea and vomiting, constipation, and heartburn.
Substitute other calcium sources for milk in her diet. Lie down after each meal. Reduce the amount of fiber she consumes. Eat five small meals daily. ANS: D. Feedback. A Incorrect: This suggestion might be appropriate for a client who is lactose intolerant; however, it will not alleviate heartburn. B Incorrect: Lying down after every meal is likely to increase the amount of heartburn that the woman is experiencing due to the position of the fetus and reflux. C Incorrect: This is an inappropriate dietary suggestion for all pregnant women, and will not alleviate heartburn. D Correct: Eating small, frequent meals may help with heartburn, nausea, and vomiting.

Developmental origins of metabolic diseases

Subject: Obstetrics and Gynecology Health Education On Postnatal Diet, PDF, Postpartum Period

Maternal Nutrition and Fetal Development - The Journal of Nutrition

Association of development quotient with nutritional status of vitamins B6, B12, and folate in 6–59-month-old children: Results from the Brazilian National Survey on Child Nutrition (ENANI-2019) - The American Journal of Clinical

Maternal Nutrition

Nutrition in pregnancy

Pregnancy: Eating Healthy for you and Your Baby Handouts and PPT Show - DOWNLOAD
Prenatal Care PowerPoint Presentation and Google Slides

Maternal Nutrition
PPT - Nutrition during Pregnancy PowerPoint Presentation, free download - ID:3086095
Pregnancy Nutrition PowerPoint Template
Maternal and Fetal Nutrition - ppt download